What is Celiac Disease?
Celiac disease is a serious autoimmune disease that occurs in genetically predisposed people where the ingestion of gluten leads to damage in the small intestine. It is estimated to affect 1 in 100 people worldwide, but only about 30% are properly diagnosed.
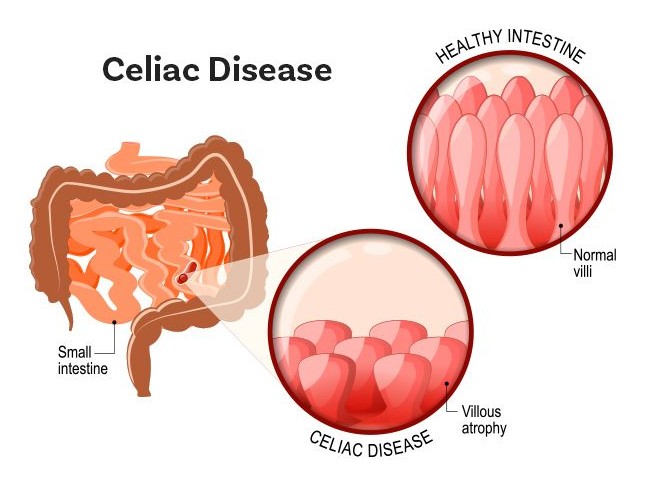
When people with celiac disease eat gluten (a protein found in wheat, rye, and barley), their body mounts an immune response that attacks the small intestine. These attacks lead to damage on the villi, small fingerlike projections that line the small intestine, that promote nutrient absorption. When the villi get damaged, nutrients cannot be absorbed properly into the body.
Celiac disease is hereditary, meaning that it runs in families. People with a first-degree relative with celiac disease (parent, child, sibling) have a 1 in 10 risk of developing celiac disease.
Celiac disease can develop at any age after people start consuming gluten. Left untreated, celiac disease can lead to additional serious health problems.
Long-Term Health Effects
People with celiac disease have a 2x greater risk of developing coronary artery disease, and a 4x greater risk of developing small bowel cancers.
The treatment burden of celiac disease is comparable to end-stage renal disease, and the partner burden is comparable to caring for a patient with cancer.
Untreated celiac disease can lead to the development of other autoimmune disorders like type 1 diabetes and multiple sclerosis (MS), and many other conditions, including dermatitis herpetiformis (an itchy skin rash), anemia, osteoporosis, infertility and miscarriage, neurological conditions like epilepsy and migraines, short stature, heart disease, and intestinal cancers.
Treatment
Currently, the only treatment for celiac disease is lifelong adherence to a strict gluten-free diet. People living gluten-free must avoid foods with wheat, rye, and barley, such as bread and beer.
Ingesting small amounts of gluten, like crumbs from a cutting board or toaster, can trigger small intestine damage.
Read about the Gluten-Free Diet.
Celiac disease is also known as coeliac disease, celiac sprue, non-tropical sprue, and gluten sensitive enteropathy.
| Early Diagnosis Lowers Chance of Developing Another Condition | |
|---|---|
| Age of Diagnosis | Chance of Developing Another Autoimmune Condition |
| 2-4 | 10.5% |
| 4-12 | 16.7% |
| 12-20 | 27% |
| Over 20 | 34% |
Undiagnosed or Untreated Celiac Disease Can Lead to:
Long-Term Health Conditions
- Early onset osteoporosis or osteopenia
- Gall bladder malfunction
- Heart disease
- Infertility and miscarriage
- Iron deficiency anemia
- Lactose intolerance
- Liver failure
- Malnutrition
- Neurological symptoms, including attention-deficit/hyperactivity disorder (ADHD), headaches, lack of muscle coordination, seizures, ataxia, dementia, neuropathy, myopathy, and multifocal leucoencephalopathy
- Pancreatic insufficiency
- Small intestine cancer and non-Hodgkin lymphoma
- Vitamin and mineral deficiencies
Other Autoimmune Disorders
In a 1999 study, Ventura, et al. found that for people with celiac disease, the later the age of diagnosis, the greater the chance of developing another autoimmune disorder.
| Autoimmune and Other Conditions Associated with Celiac Disease | |
|---|---|
| Autoimmune Condition | Prevalence in CD Population |
| Anemia | 12-69% |
| Autoimmune Hepatitis | 2% |
| Autoimmune Thyroid Disease | 26% |
| Chronic fatigue syndrome | 2% |
| Dermatitis Herpetiformis | 25% |
| Down syndrome | 12% |
| Gluten ataxia | 10-12% |
| Idiopathic Dilated Cardiomyapathy | 5.7% |
| Juveline Idiopathic Arthritis | 1.5-6.6% |
| Liver Disease | 10% |
| Lymphocytic Colitis | 15-27% |
| Microscopic Colitis | 4% |
| Peripheral Neuropathy | 10-12% |
| Primary Bilary Cirrhosis | 3% |
| Sjögren’s Syndrome | 3% |
| Type 1 Diabetes | 8-10% |
| Unexplained infertility | 12% |
Blood. 2007 Jan 15; 109(2): 412–421, Biomed Res Int. 2013; 2013: 127589, Expert Rev Gastroenterol Hepatol. 2010;4(6):767-780, PMC 2009; 55:349–365, Gut 49.4 (2001): 502-505, Ravelli, Lancet; 2007, 369(9563):767-78, Bai, et al. “World Gastroenterology Organization Practice Guidelines:.” World Gastroenterology Organization.