Inflammatory Bowel Disease and Celiac Disease Share Increased Risk
By Van Waffle
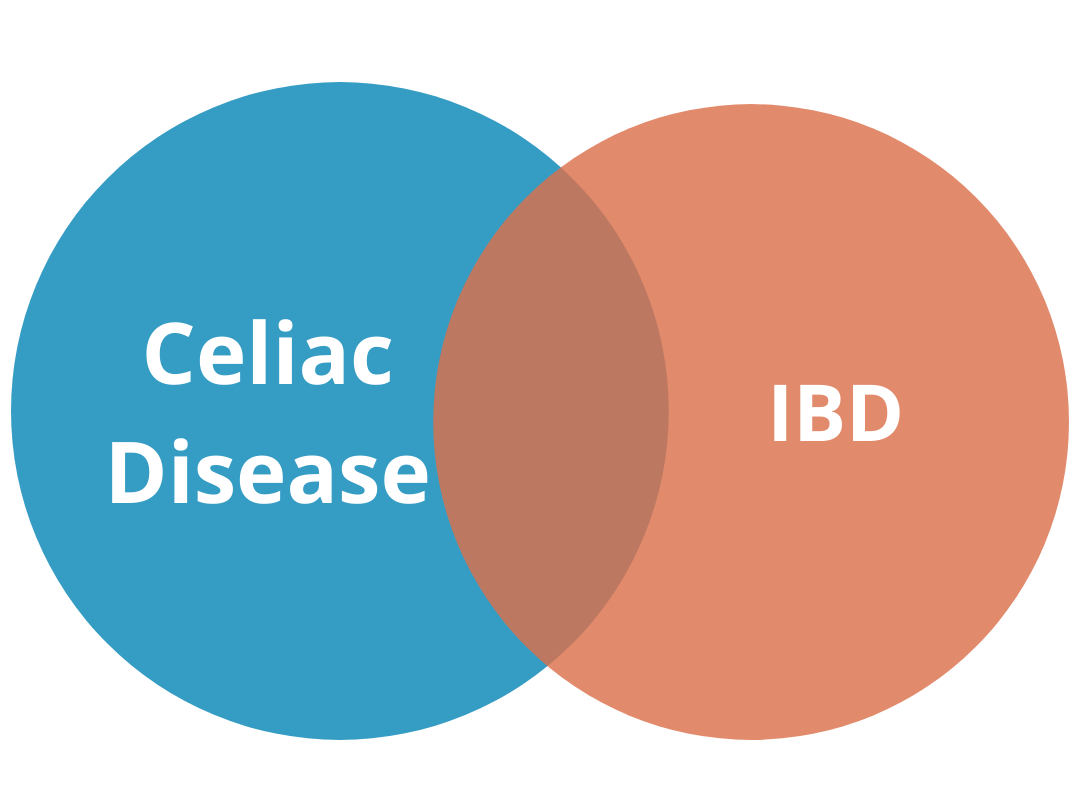
People with celiac disease have a greater risk for inflammatory bowel disease (IBD) and vice versa. A new study reviewing and analyzing all previous research about the link between these two autoimmune disorders was conducted at McMaster University, Hamilton, Canada.
“We were able to confirm for the first time ever that there is a real association between celiac disease and inflammatory bowel diseases,” says Ines Pinto-Sanchez, MD, Assistant Professor of Medicine and Clinical Leader of the Celiac Disease Clinic at McMaster Farncombe Institute. Lead author was Professor of Medicine Elena Verdú, MD, PhD.
The study recommends doctors should consider investigating an additional diagnosis to explain poor recovery in patients who are being treated for IBD or celiac disease. However, the authors stop short of recommending that patients with one of the diseases should be screened for the other. Further research is needed to show cost-effectiveness, explains Pinto-Sanchez.
People with celiac have a 10-fold greater risk for IBD, according to the study. People with IBD have a four-fold greater risk for celiac disease.
Pinto-Sanchez, who conducted the meta-analysis, says, “Evaluating the association between inflammatory bowel diseases and celiac disease was of crucial importance. There were so many different types of studies going around and still the question remained unanswered. We were not yet able to tell our celiac patients whether they have increased risk of inflammatory bowel disease, and the opposite.”
People with celiac have a 10-fold greater risk for IBD, according to the study. People with IBD have a four-fold greater risk for celiac disease.
A database search identified 9,791 relevant studies for review. Criteria such as study design narrowed it down to 65 for meta-analysis, published between 1978 and 2019. Thirty studies having control groups were pooled to calculate relative risk. These included more than 13 million people in total, 43,000 with celiac disease and 166,000 with IBD. Pinto-Sanchez says the large number of studies and population was the key to find convincing evidence.
“This systematic review confirms that these two immune-related intestinal disorders co-occur more often than chance would suggest,” says Benjamin Lebwohl, MD, Director of Clinical Research at the Celiac Disease Center at Columbia University, New York, who helped design the study and interpret findings. “While this might be in part due to increased awareness and testing, it is unlikely to wholly account for this association.”
Lebwohl cautions IBD patients considering the gluten-free diet as an alternative treatment: “It is important that people with IBD who are considering this diet first get tested for celiac disease, because once the gluten-free diet is begun, it becomes more difficult to test for this condition.”
The study raises concern that many celiac diagnoses in IBD patients may be based on false positive blood tests for anti-tissue transglutaminase (tTG), but this needs further study. Pinto-Sanchez explains that gut damage from IBD can be mistaken for celiac damage when investigated by endoscopy. IBD can also temporarily elevate tTG, considered a specific indicator for the celiac autoimmune response. Patients with other autoimmune diseases should be meticulously retested to determine whether tTG antibodies truly indicate celiac disease. However, celiac diagnosis could help some IBD patients manage their disease better using a gluten-free diet without increasing drug dosage.
More than half the eligible studies came from Europe, 39, only 12 from North America. Pinto-Sanchez points out only two came from Canada, one considering adult patients and the other children. Canada has the highest IBD prevalence of any country. It affects about 1 in 150 Canadians.
Pinto-Sanchez says the first question for further study is whether people with one disease should be tested for the other.
Source: Association Between Inflammatory Bowel Diseases and Celiac Disease: A Systematic Review and Meta-Analysis. Pinto-Sanchez, Maria Ines et al. Gastroenterology, Volume 0, Issue 0.