Nausea and Vomiting Mark Gluten Exposure in Celiac Disease
By Van Waffle
Though a promising drug failed in clinical trials last year, data from the research provides critical new insights into celiac disease. When patients are exposed to gluten, they show an immune reaction within two hours, more quickly than previously believed. Even the symptoms are different from what many expect. Robert Anderson, MD, PhD, a former lead researcher on Nexvax2, says this is a wakeup call that drug research may be testing patients the wrong way.
Most patients predicted that their worst symptoms when exposed to gluten would be classic lower digestive problems like diarrhea, bloating and cramps. However, none of these occurred during the acute immune responses observed by Anderson’s team. Instead, patients experienced nausea and vomiting. Anderson describes them as, “acute food poisoning symptoms that are early in onset,” and relatively severe.
“For all the years that we've known about celiac disease, persons have told us that they had these acute reactions, but many experts in the field dismissed them as being just in the person's mind,” says Anderson. “Here we are now, a hundred years after celiac disease was discovered, suddenly discovering, yes, the patients were right.”
“For all the years that we’ve known about celiac disease, persons have told us that they had these acute reactions, but many experts in the field dismissed them as being just in the person’s mind,” says Anderson. “Here we are now, a hundred years after celiac disease was discovered, suddenly discovering, yes, the patients were right.”
The celiac immune response involves t-cells, attack cells armed to target gluten. Specialized t-cells take time to activate. So conventional wisdom cast doubt on any symptoms appearing so quickly. However, the Nexvax2 research found evidence of immediate t-cell activity. In 92 percent of celiac patients tested, a protein, interleukin-2, spiked in the blood one hour after they ate gluten.
“Interleukin-2 almost exclusively comes from activated t-cells,” says Anderson. “Previously it had not been thought that patients could have t-cell activations that quickly, causing symptoms.”
Gluten can make people with celiac disease sick quickly, yet patients and many doctors expect to see the slow pain of cramps and diarrhea. Nexvax2 studies suggest gluten might not be to blame for those symptoms.
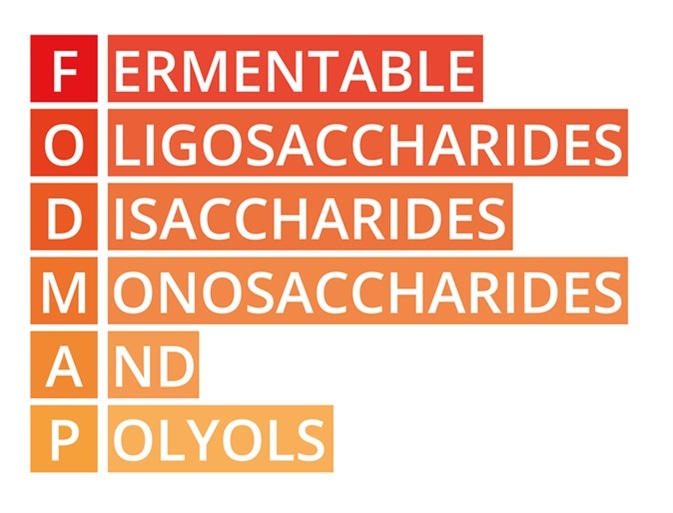
The cause might be FODMAPs, a range of short-chain carbohydrates occurring in fruits, vegetables and beans. Difficult to digest and absorb, they can ferment in the gut and trigger irritable bowel syndrome.
Fructans are a kind of FODMAP contained in grains like wheat. Symptoms can be easily misinterpreted because a slice of wheat bread contains both gluten and FODMAPs. In fact, some celiac clinical trials treat patients to a gluten challenge by feeding them wheat flour.
Nexvax2 trial eliminated FODMAPs altogether. Patients received food samples that contained either six grams of gluten or a gluten-free sham for comparison. All were low in FODMAPs. The procedure practically eliminated symptoms of irritable bowel syndrome from the picture. The results were clear: nausea and vomiting accompany acute immune reaction when people with celiac disease eat gluten.
“I hope that if people recognize nausea and vomiting are the symptoms of gluten exposure, they will also understand that other symptoms they experience are probably due to something else, in particular FODMAPs."
Anderson describes six grams as “quite a hefty amount of gluten.” For comparison, a slice of wheat bread contains between two and four grams. This is much more than a celiac patient would accidentally consume from careless cross-contact in a restaurant, which might not cause any symptoms at all. Nausea within two hours after eating appears the most reliable indicator of substantial gluten intake.
People with celiac disease who experience persistent abdominal discomfort may miss the mark if they blame it on accidental gluten. The study suggests patients with symptoms like cramps and diarrhea should discuss them with a doctor as they might implicate irritable bowel syndrome or other conditions.
Anderson says these findings signal a critical time in celiac drug research: “If we are trying to develop drugs for symptoms that aren’t directly due to gluten, then it’s likely we will fail. You may develop a drug that could treat irritable bowel syndrome, but it’s not addressing the cause of celiac disease.”
The current approach is unlikely to get a drug approved for celiac disease, Anderson says. He calls for more work to correlate the correct symptoms with the immune response to gluten. The good news is a marker like interleukin-2 could speed up research. Instead of tracking patients’ gluten exposure for weeks or months, drug trials could use a simple blood test to monitor a patient’s single exposure to gluten.
After Nexvax2 trials halted in the United States, Anderson returned home to Brisbane, Australia, where he is working with Coral Sea Clinic Research Institute setting up independent research in celiac disease. A study of key celiac symptoms in Alimentary Pharmacology and Therapeutics is one of several derived from the Nexvax2 trial and published recently.
Want to confirm that your symptoms are related to gluten exposure? Gluten Detective is an easy to use at-home test to detect gluten fragments in stool and urine samples. Use the Gluten Detective test to determine if your symptoms might have been triggered by gluten and not other food sensitivities like FODMAPs. Click here to learn more and order your test kit today!
Add your data to our iCureCeliac® patient registry today. iCureCeliac® is a free online portal for patients, or their caregivers, to provide critical insights into life with celiac disease. Your participation will help create better diagnostic tools and treatments for cross-contact and gluten consumption, governmental policy changes, and access to new and innovative clinical trials nationwide, which may, one day, cure celiac disease.